Uncovering the Connection Between PCOS and Menstrual Disorders
Polycystic Ovary Syndrome (PCOS), perimenopause, and menstrual disorders are common gynaecological conditions that affect a significant number of women globally. Each condition presents unique symptoms and health implications, necessitating precise diagnostic criteria and comprehensive management strategies. Recent advancements emphasise the refinement of diagnostic criteria, simplified diagnostic algorithms, and the inclusion of anti-Müllerian hormone (AMH) levels as an alternative to ultrasound in diagnosing PCOS. Additionally, there is a growing focus on recognising the broader features of PCOS, mainly its association with metabolic and cardiovascular risks.
What is Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder commonly affecting women of reproductive age. The WHO estimates that PCOS affects an estimated 8-13% of women of reproductive age, and the same publication estimated that up to 70% of such cases remain undiagnosed.
Women with PCOS often have elevated levels of androgens, a male sex hormone. In some cases, patients with PCOS don’t produce enough female sex hormones, leading to irregular menstrual cycles, excessive hair growth, acne, and weight gain. Here are some of the telltale signs of PCOS:
- Irregular Menstrual Cycles: One of the telltale signs of PCOS is irregular menstrual periods, which result from hormonal imbalances preventing regular ovulation.
- Excessive Hair Growth and Acne: High levels of androgens can lead to hirsutism—unwanted male-pattern hair growth on the face, chest, and back. Acne is also commonly seen on the face, chest, and upper back.
- Weight Gain: Many women with PCOS often experience rapid weight gain due to the hormonal shifts often associated with PCOS.
- Oily Skin or Dandruff: Changes in skin oil production can lead to dermatological issues, including dandruff or oily skin.
Diagnostic Criteria
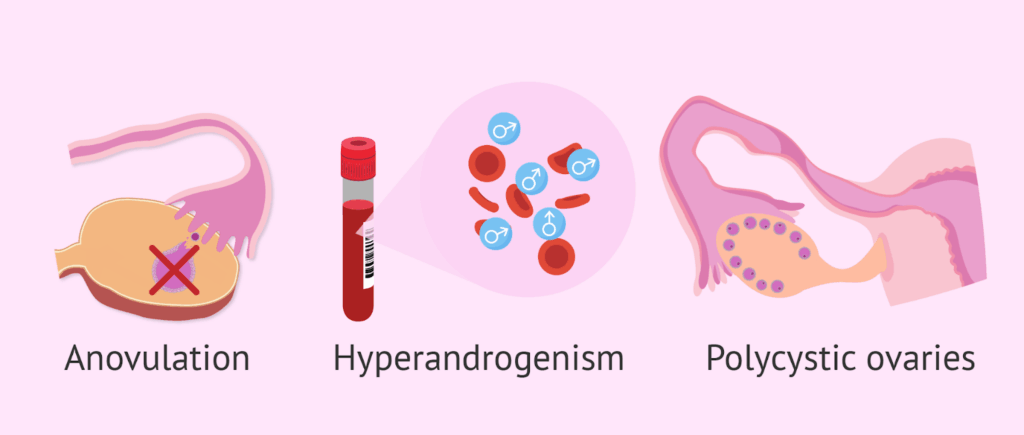
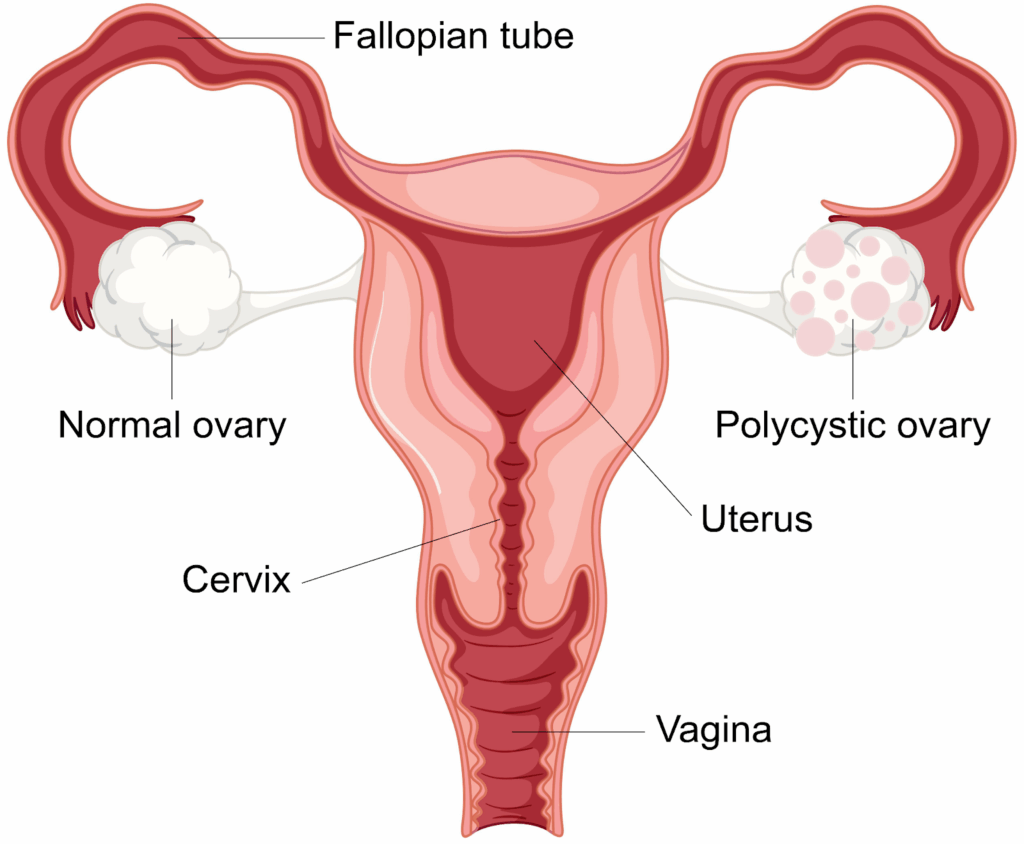
The Rotterdam criteria is the gold standard for diagnosing PCOS. As per the Rotterdam method, the identification of PCOS requires the presence of at least two of the following three features:
- Oligo- or anovulation (irregular or absent menstrual periods)
- Indications of hyperandrogenism (including hirsutism, acne, or elevated androgen levels in blood tests)
- Polycystic ovaries (usually found when performing ultrasound scan)
However, recent studies suggest refining these criteria by incorporating Anti-Mullerian Hormone (AMH) levels as an alternative to ultrasound, particularly in adults. Ultrasound is not always reliable for diagnosing PCOS because it may not consistently detect the small cysts on the ovaries, which are a hallmark of the condition. Additionally, the presence of polycystic ovaries alone is not sufficient for a PCOS diagnosis, as many women without PCOS can have polycystic ovaries. The variability in ultrasound results and the overlap of ovarian cysts with other conditions can lead to misdiagnosis or overdiagnosis.
AMH is a hormone produced by the ovarian follicles and is often tested to measure ovarian reserve. Recent studies have found that women with PCOS typically have higher AMH levels due to the increased number of small, undeveloped follicles that secrete the hormone. A recent study performed by the Department of Endocrinology at China Medical University suggests that serum AMH levels in PCOS cases are usually 2-3 times higher than in average women without PCOS. As such, measuring AMH levels can be a good indication of PCOS if performed alongside the traditional Rotterdam diagnostic criteria of anovulation or measurement of androgen levels.
Risk Factors
Polycystic Ovary Syndrome (PCOS) is more common among Asian women compared to other ethnic groups due to a combination of factors. An extensive study published at the National Center for Biotechnology Information indicates that South Asian women, in particular, exhibit higher prevalence rates of PCOS, and their symptoms tend to be more severe.
- Genetic Factors: Studies have shown that genes associated with insulin resistance and elevated androgen production are more prevalent among Asians. These genetic factors contribute to the development and severity of PCOS symptoms.
- Lifestyle Factors: Diet and lifestyle also significantly impact the prevalence of PCOS among Asian women. Traditional diets high in refined carbohydrates and low in fibre, combined with a sedentary lifestyle, contribute to obesity and insulin resistance. Additionally, cultural and societal factors may influence health-seeking behaviour and the management of PCOS, leading to delayed diagnosis and treatment.
Broader Features and Metabolic Risks
Due to the hormonal imbalances associated with it, PCOS is not only a reproductive disorder but also has significant metabolic implications. Here are some of the most common metabolic associations of PCOS:
- Insulin Resistance and Type 2 Diabetes: Insulin resistance is a common complication of PCOS; Individuals with insulin resistance are at higher risk of developing Type 2 Diabetes.
- Obesity: Many women with PCOS struggle with weight management, which can exacerbate metabolic and cardiovascular risks.
- Cardiovascular Disease: PCOS is associated with an increased risk of cardiovascular diseases, including hypertension, dyslipidemia, and atherosclerosis.
- Mood swings and depression
Correlation between Common Menstrual Disorders and PCOS
The correlation between PCOS and menstrual disorders is well-established, with irregular, heavy, or absent menstrual cycles being common symptoms. These menstrual irregularities are primarily due to the hormonal imbalances and metabolic disturbances characteristic of PCOS. Here’s an overview of some common menstrual disorders and its link to PCOS:
- Dysmenorrhea (Painful Periods): This involves severe, often debilitating cramps during menstruation; it might be accompanied by nausea, vomiting, fatigue, and diarrhoea.
- Heavy Periods (Menorrhagia): When women with PCOS do menstruate, they may experience heavy menstrual bleeding (menorrhagia). This is due to the prolonged buildup of the endometrial lining, which occurs when ovulation is infrequent or absent, causing heavier bleeding when menstruation finally occurs.
- Light or Absent Periods (Oligomenorrhea and Amenorrhea): Due to elevated levels of androgens and other hormonal imbalances, women with PCOS often experience oligo-ovulation or anovulation, which means they ovulate infrequently or not at all. This leads to irregular, infrequent, or absent menstrual periods (oligomenorrhea or amenorrhea).
Perimenopause Period for Women with PCOS
Polycystic Ovary Syndrome (PCOS) can lead to delayed menopause due to the hormonal imbalances associated with the condition. Women with PCOS typically have higher levels of androgens and a greater number of ovarian follicles compared to those without the condition. This increased ovarian reserve, indicated by elevated levels of anti-Müllerian hormone (AMH), can prolong ovarian function and delay the onset of menopause.
Apart from delayed menopausal period, women with PCOS will often experience the following symptoms upon their perimenopausal transition:
- Hormonal Changes: Hormonal imbalances, which are often associated with PCOS, can worsen during perimenopause. This imbalance will cause more severe symptoms for women with PCOS when entering perimenopause
- More pronounced menstrual irregularities
- Elevated metabolic risks: Metabolic risks associated with PCOS can persist and increase during perimenopause due to the natural ageing process and hormonal changes.
Treatment Plans for PCOS and Related Disorders
If you have PCOS or suspect you may have it, it’s important to seek care from an endocrinologist. Early diagnosis and tailored treatment plans from a specialist can help manage symptoms more effectively and prevent complications such as type 2 diabetes, cardiovascular disease, and fertility issues. With the right guidance and treatment, you can significantly improve your long-term health outcomes.
According to Dr Vikram Sonawane, while there is no cure for PCOS, there are several treatment plans which can improve its symptoms and reduce the risks of other complications. These include:
Lifestyle modifications: Diet and exercise are fundamental components of PCOS management. A balanced diet low in processed carbohydrates and high in fibre combined with regular physical activities will help reduce insulin resistance and improve weight management, which is crucial for alleviating PCOS symptoms.
Medications: Certain types of contraceptives, such as birth control pills, help reset the menstrual cycle and control androgen hormone levels.
Infertility treatments: For those struggling with infertility, treatments like letrozole, gonadotropins, or assisted reproductive technologies (ART), such as in vitro fertilisation (IVF), may be recommended.
Summary
PCOS, perimenopause, and menstrual disorders are common but complex conditions that require careful diagnosis and management. Recent advancements in diagnostic criteria, including measuring AMH levels, have simplified identifying PCOS. Recognising the broader features of PCOS, particularly its metabolic and cardiovascular risks, is crucial for comprehensive care. Understanding the symptoms and management strategies for perimenopause and menstrual disorders further enhances women’s health and quality of life. With ongoing research and improved diagnostic tools, healthcare providers can offer more effective and personalised care to women affected by these conditions.
If you or your loved ones are suffering from polycystic ovary syndrome, menstrual disorders and perimenopause, you can schedule an appointment with our Senior Consultant Endocrinologist, Dr Vikram from Harmony Thyroid, Endocrinology, and Diabetes Centre.
References:
- Guo L, Gordon NP, Chandra M, Dayo O, Lo JC. The Risks of Polycystic Ovary Syndrome and Diabetes Vary by Ethnic Subgroup Among Young Asian Women. Diabetes Care. 2021;44(6):e129-e130. doi:https://doi.org/10.2337/dc21-0373
- Polycystic ovary syndrome. www.who.int. Accessed July 12, 2024. https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome?gad_source=1&gclid=CjwKCAiA6KWvBhAREiwAFPZM7scpschvJakb3T8VNtFP4XEaWFUu6vmTqxSxw0Il72ZG292TvuLqcxoC7fkQAvD_BwE
- Saxena U, Ramani M, Singh P. Role of AMH as Diagnostic Tool for Polycystic Ovarian Syndrome. The Journal of Obstetrics and Gynecology of India. 2017;68(2):117-122. doi:https://doi.org/10.1007/s13224-017-1066-4
- Zhao H, Zhou D, Liu C, Zhang L. The Relationship Between Insulin Resistance and Obesity and Serum Anti-Mullerian Hormone Level in Chinese Women with Polycystic Ovary Syndrome: A Retrospective, Single-Center Cohort Study. International Journal of Women’s Health. 2023;Volume 15:151-166. doi:https://doi.org/10.2147/ijwh.s393594

